ICU Management & Practice, Volume 16 - Issue 1, 2016
Since its first clinical use in the 1950s, the set-up and management of the heart-lung machine (HLM) has been the responsibility of the perfusionist, who has a documented competency in every facet of extracorporeal technology because of their theoretical and practical training. In contrast, when this technology leaves the operating room to provide longer-term support in terms of ECLS (extracorporeal life support) or ECMO (extracorporeal membrane oxygenation), there is no longer worldwide uniformity nor consensus concerning clinical roles or responsibilities. It is clear that certain involvement from the extracorporeal technology specialists is required to provide quality ECMO care, but the extent of their involvement has been undefined within Europe. As it was unclear how intensely perfusionists around Europe are involved in ECLS, a survey was created inquiring about their roles and responsibilities in local ECMO programmes.
Staffing Roles in ECMO Programmes – Historical Growth
ECLS systems are composed of mechanical devices designed to temporarily take over the pump function of the heart and gas exchange function of the lungs. Although based on the same technology as the HLM, which is used during open heart surgery, these ECLS devices have different features to enable more long-term support and to allow more distant supervision. Many ICUs have started an ECMO programme with various success, depending on the indications but also on their training, expertise and type of multidisciplinary collaboration (Paden et al. 2014).
The term “ECMO specialist” was introduced in the U.S., referring to the person specialized in taking care of the patient on ECMO, and each institution had its own unique training for these individuals. In a 2008 survey of North American ELSO centres’ team roles, it was identified that these ECMO specialists came from a variety of departments; they were nurses, respiratory therapists, perfusionists or physicians. The degrees of involvement of perfusionists varied depending on their ability to handle both cardiac surgical cases and ECMO cases outside the operating room, and therefore other disciplines were forced to take over some of the roles perfusionists were trained for so intensely. It was not uncommon that in respiratory ECMO centres nurses were trained to become ECMO specialists, while cardiac ECMO remained mostly under the supervision of the perfusionist (Lawson et al. 2008).
To provide support to institutions delivering ECLS, the Extracorporeal Life Support Organization (ELSO) was founded in the USA in 1989. ELSO has established an observational data registry, offers a platform supporting education, training and research, provides practice guidelines and organises international ECMO meetings. Broad multidisciplinary participation is strongly encouraged by ELSO without identifying or defining responsibilities (elso.org).
Within Europe, ECMO as an adjuvant therapy in both respiratory and cardiac support remained controversial for many years, especially as no evidence of superiority above conventional treatment was found in the few randomized trials, except in neonatal respiratory ECMO. Only due to the isolated successes reported in case series were there ongoing but variable efforts to place patients on ECMO, mostly when the entire treatment arsenal was exhausted. Thanks to the reappraisal of ECMO as a temporary solution in patients in cardiac failure, and with the positive outcome of the Cesar trial in adult respiratory failure (Peek et al. 2009), centres started to reconsider putting patients on ECMO. The Influenza A (H1N1) pandemic pushed many who were still considering over the edge and since 2009 we have experienced a boom in ECMO in ICUs all over Europe (Paden et al. 2014).
Because of the struggling growth and also because of the regulatory and historical differences with the U.S., not many centres within Europe were initially interested in joining ELSO. With the rapidly growing interest in ECMO in the last few years, a European chapter of ELSO (EuroELSO) was founded in 2011 to offer more relevant support and a platform for European ECMO centres. Since the establishment of EuroELSO, the registration of European centres has rapidly grown (Fig. 1). 78 European ECLS centres from all over Europe are registered and can seek ELSO support (2015 figure).

Perfusionists’ Role in ECLS Centres –Results of a European Survey
To identify how intensely perfusionists around Europe are involved in ECLS programmes, a survey was created with SurveyMonkey (Vercaemst 2015). The survey was sent, starting in May 2014, to the delegates of all European countries that are members of the European Board of Cardiovascular Perfusionists (EBCP) with the request to forward it to the Perfusion Department of each cardiac surgery centre within their country. There was a good response overall from all over Europe; apart from Greece and Spain, who had some problems forwarding the survey towards their ECLS units, all EBCP countries responded (Fig. 2).

A total of 199 centres from 20 countries responded to the survey; of the responding centres 70% had an active ECLS programme; nearly 20% intend to start in the near future.
Only the current 135 and 34 ECLS centres starting in the near future were asked to complete the entire survey.
Asked if their centres are ELSO-registered,only 23% could confirm and only 14% were aware of their data being sent to the ELSO Registry (Fig. 3).

The main reason for this limited involvement seems to be lack of information about EuroELSO and its Data Registry and lack of awareness concerning its value in daily practice. Some respondents also expressed the concern for needing patient consent to be legally allowed to submit data.
All active and future centres were first asked a few questions concerning size and type of their centre (Fig. 4 & 5), and the answers indicated that ECMO remains an infrequently instituted therapy thus making it hard to gain routine experience and expertise.


The answers to the survey questions concerning clinical roles (Fig. 6 & 7) revealed the important clinical involvement overall of perfusionists—from setting up and priming the circuit until weaning off the ECLS. In nearly 20% of centres, the perfusionist remained bedside 24/24hrs to monitor the circuit. Many centres started up an ECMO programme while experiencing a busy cardiac surgery programme, hence the restrictions some centres have in making perfusionists available outside the operating room.


If not present at the bedside 24/24hrs, the perfusionist visits the ECMO patient on a regular basis to check the circuit and optimise circuit settings. Also for technical troubleshooting a perfusionist is available 24/24.
In most European ECLS centres, physicians are clearly participating in some tasks, while nurses’ roles remain limited to patient rounds and data entry. In contrast to the U.S., there seems to be little involvement of the so-called ‘ECMO specialists’ or at least this terminology is not adapted by many European centres. Only very few centres indicated the involvement of an ECMO specialist, and those who did were asked to define the background of this person. In half of these cases this referred to an “ICU nurse with a specialty ECMO training”; the other half referred to “Perfusionists with extensive experience in ECMO”.
Most centres report the same involvement of perfusionists in cardiac as in respiratory ECMO, but it is unclear who takes this involvement in the non-cardiac surgery centres without perfusionists as these centres were not addressed for the survey (Fig. 8).

In many countries there seem to be no legal restrictions in
setting up cardiac or respiratory ECMO programmes, hence the reason for the increased
amount of small ECMO volume centres all over Europe (Fig. 9).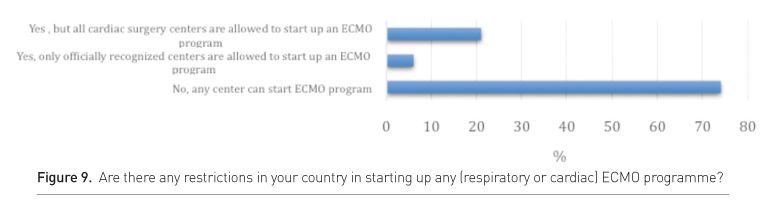
The majority of centres stated that additional training for perfusionists, physicians and nurses should be compulsory before starting up an ECMO programme and also that there should be support from an expert ECLS centre.
Most perfusionists agreed that there should be “Minimum Standards of Care’” established to which all ECLS centres should adhere. These Minimum Standards of Care would be written minimum requirements concerning staffing, training, experience, equipment, safety and so on, in order to optimise quality of ECLS programmes.
Discussion
From the results of the survey, it is clear that perfusionists within Europe have an important involvement in their in-house ECMO programme. There seems to be a variety of responsibilities once ECMO is initiated, but unlike in the U.S. there is little mention of nurses or ECMO specialists involved in the technical part of the ECMO programme.
The survey did not address the isolated respiratory ECMO programmes, which are set up in hospitals without a cardiac programme, so it is unclear who takes over the technical support in those centres. Isolated respiratory units experience more difficulties setting up a quality ECLS programme, as the absence of a cardiac surgery programme is a significant barrier to the development of an ECLS programme. There are such centres that have successfully initiated an ECMO programme with a smooth learning curve, but they need a well-organised, intensive and interdisciplinary training curriculum with well-defined roles and responsibilities (Sanchez- Glanville et al. 2015).
The survey also did not address non-specialised, peripheral centres putting their in-house patients on urgent ECLS with the help of a trained in-house or external team. It is not sufficient to have a trained physician to place the cannula and a specialist to prepare the circuit and initiate the ECMO therapy. The most challenging part is not to initiate, but to wean from ECMO, which can only be achieved if the failing organs are allowed to recover while providing efficient support. If physicians choose to start an ECMO treatment in a non-specialised centre, they owe it to the patient to transport him or her to an ECMO specialist centre for specialized supervision and optimal multidisciplinary care (Combes et al. 2014).
Whether 24/24hrs bedside technical support is needed depends upon the availability of a perfusionist, but also upon the experience and knowledge of the bedside caregiver. Staffing models in experienced centres with good outcomes prove that with the right training, it is possible to give safe and quality care to the patient on ECMO without a bedside perfusionist, on condition that there is a 24/24hrs on-call service for technical backup (Beckmann et al. 2011). Ideally, ongoing practical training with simulation training should be part of the training curriculum so that in the worst case scenario, telephone guidance should be sufficient to assist the bedside caregiver for urgent troubleshooting.
Staffing models might also differ depending on the volume of ECMOs performed. Recent data demonstrated significant better outcomes in centres which perform more than 20-25 cases a year as opposed to those with fewer than 20 ECMO cases a year (Combes et al. 2014). Maintenance of technical skills might be difficult in the low volume centres, and here a more close cooperation with the perfusionist is required to maintain a safe and quality ECMO programme (Mongero et al. 2013).
Larger centres still report a significant number of ECLS-related complications, so there is still room for improvement (ELSO 2016). Not only survival but most importantly quality of life should be the focus. Support-related complications must be kept as low as possible. Late diagnostics of failing circuit parts often cause hazardous and complicated change-outs. Support needs to be evaluated on a continuous basis as inefficient support can be detrimental for the patients. Taking over too little ventricular function can result in multi-organ failure while seemingly sufficient support can destroy the patient’s left ventricle permanently. Aggressive forces can lead to blood cell destruction with toxic end products, and anticoagulation disturbances can clot off the circuit or cause patient bleeding. These are only a few examples of complications, which can be minimized with trained bedside personnel supervising the patient.
ELSO recommends the assignment of an ECMO director to take medical responsibility for the programme and an ECMO coordinator to assist the ECMO director in safeguarding the quality of the programme. The role of ECMO coordinator is an important role requiring an intensive commitment, which might not be possible for all team members. In 2014, from the 81 European ELSO registered centres, 6 ECMO coordinators were certified perfusionists, 49 were medical doctors and most of the remaining 26 were registered nurses (Vercaemst 2015). Depending on the size of the ECMO programme, the job of the coordinator might require different investments, but there needs to be some official time allocation for whoever is assigned this job.
Conclusion
1. There is no standard of care that addresses ECLS personnel, training and programme structures, but it is clear that a successful ECLS programme needs multidisciplinary involvement, guidelines and defined roles.
2. ECLS circuitry is complex both in set-up and in major troubleshooting and therefore should remain the responsibility of the perfusionist. European perfusionists play an important, mainly technical supportive role in local ECLS programmes, but rarely offer a 24/24hrs bedside service, hence the importance of a well-trained bedside caregiver.
3. It is essential and beneficial for the patients’ total approach that everyone on the team receives specialised training about all aspects of ECLS. As extracorporeal support technologies are the core business of perfusionists, technical training should ideally be provided by the perfusionist.
4. Each ECMO centre aiming at quality care should appoint an ECMO coordinator to assist the medical ECMO director with organising and implementing the training of the ECMO team, staffing, team meetings, quality improvement, protocol writing, maintaining equipment and supplies, and ensuring that data are entered into a database.
5. There are still many ECMO-related complications reported, so in-house data should be evaluated on a regular basis and preferably be benchmarked against the outcomes of experienced centres. Worrying results should be analysed and expert advice should be sought.
6. European ECLS programmes still lack involvement in ELSO,
which offers important support to ECMO centres.
Abbreviations
EBCP European Board of Cardiovascular Perfusion
ECLS extracorporeal life support
ECMO extracorporeal membranc oxygenation
ELSO Extracorporeal Life Support Organization
HLM heart-lung machine




















